enfants diabétiques
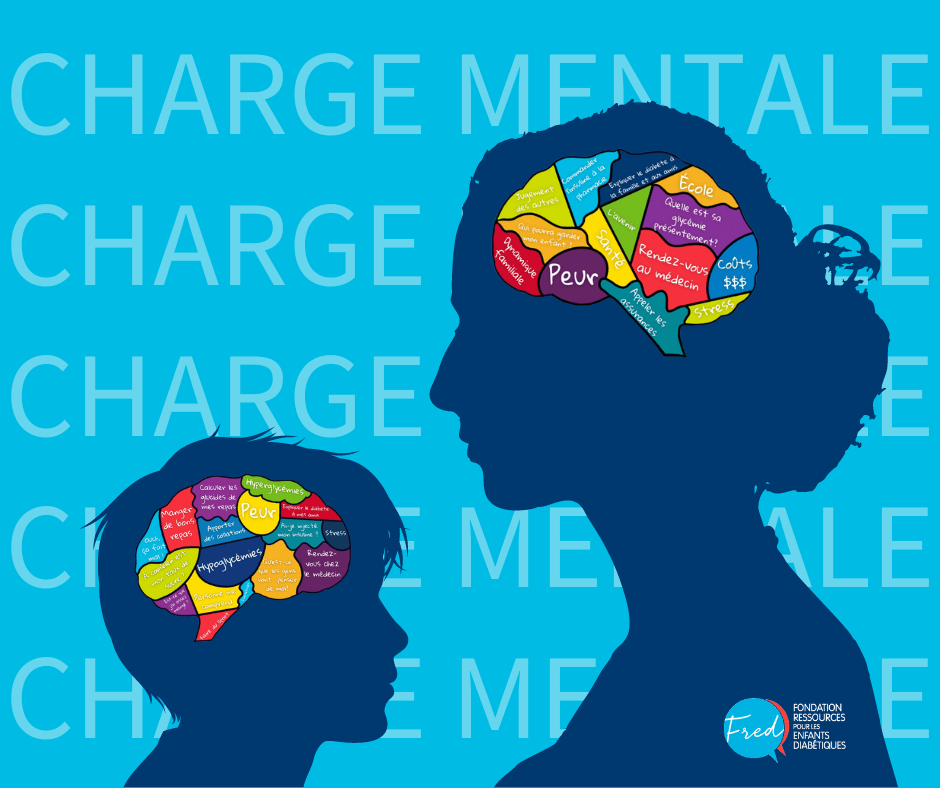
Fred rassemble les ressources nécessaires pour améliorer le quotidien des enfants et des familles vivant avec le diabète de type 1 au Québec. Fred réunit les familles, les professionnels de la santé, la société, la communauté de soutien, la science et l’éducation.
4 000
DT1 au Québec.
2 820
auprès de Fred.

150+
s’inscrivent chez Fred
tous les ans.
300
Camp Carowanis
chaque année.

4 000
DT1 au Québec.
2 820
auprès de Fred.
150+
s’inscrivent chez Fred
tous les ans.
300
Camp Carowanis
chaque année.

S'informer avec Fred
Demandez votre
trousse d’accompagnement
s'amuser avec fred
Prochaines activités
à venir
Fred crée des communautés grandissantes de soutien afin de favoriser la communication entre les parents et les enfants en offrant des opportunités amusantes d’échanges qui motivent l’inclusion et qui permet de démystifier la maladie tout en redonnant confiance aux enfants dans leur milieu.


Vous souhaitez recevoir des conseils, des outils, des invitations exclusives à nos événements éducatifs et sociaux et ainsi partager avec des gens qui vivent les mêmes défis que vous, et ce, sans frais ni obligation ?


J’organise une
levée de fonds
de l’espoir aux enfants DT1.


J’organise une
levée de fonds
de l’espoir aux enfants DT1.

Un camp d’été unique au Québec pour les
jeunes diabétiques de 7 à 16 ans
Depuis 1958, le Camp Carowanis offre une expérience de camp de vacances spécifiquement adaptés aux jeunes diabétiques au coeur de la forêt qui borde le lac Didi à Ste-Agathe-des-Monts. Un endroit où se créé une panoplie de souvenirs, de belles amitiés et où la différence n’a aucune limite. C’est aussi un camp avec une programmation d’activités diversifiés qui donneront des outils pour la vie à votre jeune DT1.
Mon espace
professionnel
Fred met en place des outils spécialisés qui permettent aux professionnels de s’impliquer auprès des jeunes, de partager des conseils et d’échanger entre eux. Ensemble, nous pouvons apporter plus de ressources et mieux soutenir les enfants DT1.